What is Crohn's disease?
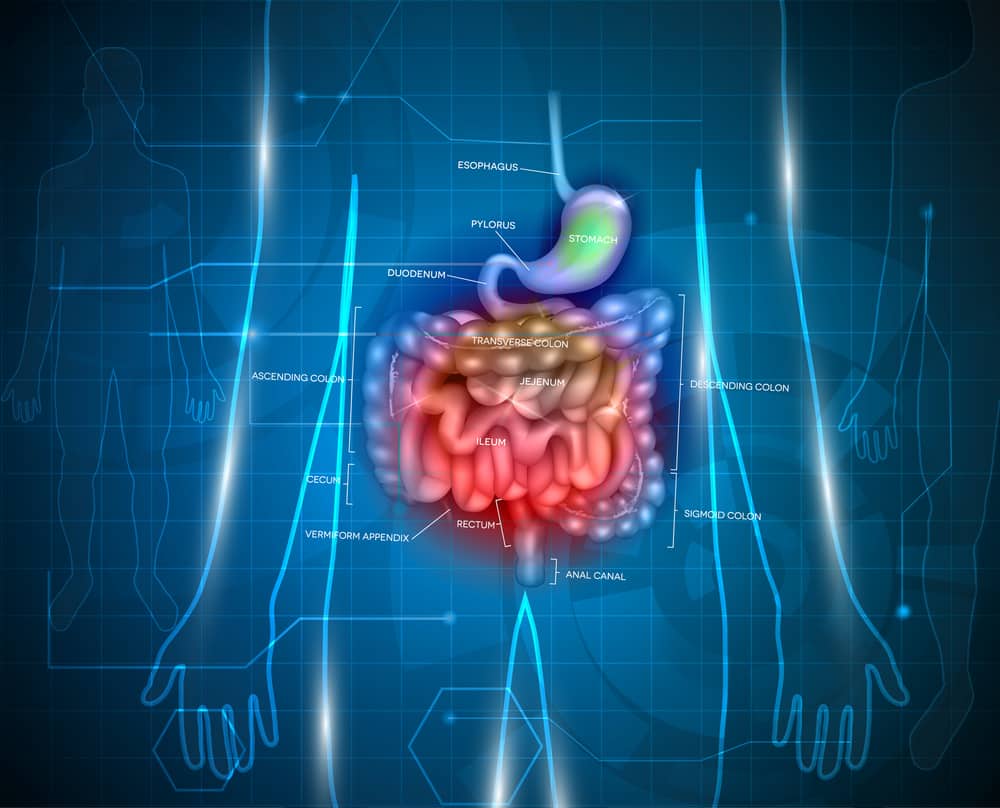
Crohn’s disease is classified as an inflammatory bowel disease, or IBD, in which any part of the gastrointestinal (GI) tract becomes inflamed. Most typically, inflammation occurs at the ileum, the end of the small intestine, where it meets the colon; however, Crohn’s disease can affect any of the GI tract from the mouth to the anus and can appear in patches.
It’s important to note that IBD is different than IBS (inflammatory bowel syndrome). IBS is not characterized by inflammation like IBD – instead, it affects muscle contractions of the bowel and is not a chronic disease.
It’s important to note that IBD is different than IBS (inflammatory bowel syndrome). IBS is not characterized by inflammation like IBD – instead, it affects muscle contractions of the bowel and is not a chronic disease.
Who can get Crohn's disease?
It is still unknown what exactly causes Crohn’s disease, but there are some factors that may play a role in development of the disease, including autoimmune reaction (bacteria in the GI tract triggering the immune system to respond with inflammation), genes (having a family member with Crohn’s disease), and factors such as taking NSAIDs/antibiotics/birth control pills, smoking, and eating a high-fat diet could increase chances of developing Crohn’s disease but do not directly cause the disease.
While Crohn’s disease is not considered a genetic disorder, about 20 percent of people with diagnosed Crohn’s disease have a blood relative who also has an IBD (even if it is not specifically Crohn’s disease).
It is estimated that over half a million people in the United States have Crohn’s disease, and has actually become more common over time in the US and other countries (specifically, urban and industrialized areas). Crohn’s disease affects men and women at the same rate, and onset can happen at any age; however, typically it started between ages 15 and 35. Symptoms range from mild to severe in those diagnosed with Crohn’s disease.
While Crohn’s disease is not considered a genetic disorder, about 20 percent of people with diagnosed Crohn’s disease have a blood relative who also has an IBD (even if it is not specifically Crohn’s disease).
It is estimated that over half a million people in the United States have Crohn’s disease, and has actually become more common over time in the US and other countries (specifically, urban and industrialized areas). Crohn’s disease affects men and women at the same rate, and onset can happen at any age; however, typically it started between ages 15 and 35. Symptoms range from mild to severe in those diagnosed with Crohn’s disease.
Signs and Symptoms
Typically, symptoms develop gradually; however, sometimes they come on suddenly. Sufferers of Crohn’s disease may also have a time period with no signs or symptoms, and this is known as remission. These periods can last weeks or even years, and 67 percent of those in remission are expected to have a relapse within the next five years.
Symptoms vary depending on where the inflammation occurs in the GI tract, but some of the common symptoms of Crohn’s disease include:
Severe symptoms and complications of Crohn’s disease include:
Symptoms vary depending on where the inflammation occurs in the GI tract, but some of the common symptoms of Crohn’s disease include:
- Diarrhea
- Fever
- Fatigue
- Pain and cramping in the abdomen
- Blood in the stool
- Reduced appetite resulting in weight loss
- Red, tender bumps under the skin
- Joint pain and soreness
Severe symptoms and complications of Crohn’s disease include:
- Inflammation of the liver or bile ducts
- Intestinal obstruction
- Fistulas from inflammation that can become infected
- Abscesses
- Anal fissures
- Ulcers (or open sores) in the mouth, intestines, anus, or perineum
- Malnutrition
- Inflammation in other body parts, such as the eyes, skin, and joints
- Colon cancer, since Crohn’s disease can increase the risk of developing colon cancer
Diagnosis
It is recommended to see a doctor with certain signs and symptoms to be checked for Crohn’s disease:
There is no one definitive test for Crohn’s disease – instead, other diseases can be ruled out through testing and then a combination of tests will be used to diagnose Crohn’s disease. Blood tests look for anemia/infection, and your stool will be checked for blood.
Other procedures to diagnose Crohn’s disease include a colonoscopy (including biopsy of colon tissue) to check for inflammation, a CT (computerized tomography) scan that looks at the entire bowel and tissues around it or an MRI to check for fistulas, a capsule endoscopy (swallowing a capsule with a camera in it then exits the body in the stool), or a balloon-assisted enteroscopy to look in the small bowel where endoscopes can’t reach.
- Unexplained abdominal pain
- Blood in the stool
- Bouts of diarrhea that are not fixed by OTC medications
- Unexplained fever that lasts longer than two days
- Unexplained weight loss or appetite changes
There is no one definitive test for Crohn’s disease – instead, other diseases can be ruled out through testing and then a combination of tests will be used to diagnose Crohn’s disease. Blood tests look for anemia/infection, and your stool will be checked for blood.
Other procedures to diagnose Crohn’s disease include a colonoscopy (including biopsy of colon tissue) to check for inflammation, a CT (computerized tomography) scan that looks at the entire bowel and tissues around it or an MRI to check for fistulas, a capsule endoscopy (swallowing a capsule with a camera in it then exits the body in the stool), or a balloon-assisted enteroscopy to look in the small bowel where endoscopes can’t reach.
Treatment
There is no cure for Crohn’s disease, and no one treatment works on everyone. Since Crohn’s disease is caused by inflammation, the goal of treatment is to reduce the inflammation that causes the symptoms and keep the patient in remission.
Medications to help treat Crohn’s disease include:
To help with the malnutrition that can result from Crohn’s disease, a doctor may provide a special diet that could be via a feeding tube or nutrient injection to give the bowel time to rest (and heal) and improve nutrition. A low fiber diet may be recommended to reduce intestinal blockage. A diet to help treat Crohn’s disease will likely also limit dairy, fat, and any other problem foods (such as caffeine, alcohol, or spicy food).
Finally, surgery may be used to help relieve complications and symptoms. About 60 percent of those with Crohn’s disease had surgery within two decades of being diagnosed with the disease. Surgery may be used to treat fistulas, life-threatening bleeding, intestinal obstructions, and other symptoms. A surgeon may remove a damaged portion of the GI tract then reconnect the sections that are still healthy. Typically, the surgery results are only temporary since the disease will cause flare ups again, often near the reconnected tissue.
Lifestyle factors including stress management, regular exercise, and relaxation techniques won’t help the disease, but could help deal with the symptoms.
Medications to help treat Crohn’s disease include:
- Aminosalicylates: help control inflammation for those newly diagnosed with mild symptoms
- Corticosteroids: steroids that reduce immune system efforts causing inflammation for those with moderate to severe symptoms
- Immunomodulators: these also reduce immune system activity to reduce inflammation
- Biologic therapies: intended to neutralize proteins created by the immune system to decrease inflammation
- Antibiotics: to help infections such as fistulas
- Loperamide: to help reduce diarrhea and only taken for a limited time
- Pain relievers such as acetaminophen (but not any NSAIDs) just for the purposes of pain management
To help with the malnutrition that can result from Crohn’s disease, a doctor may provide a special diet that could be via a feeding tube or nutrient injection to give the bowel time to rest (and heal) and improve nutrition. A low fiber diet may be recommended to reduce intestinal blockage. A diet to help treat Crohn’s disease will likely also limit dairy, fat, and any other problem foods (such as caffeine, alcohol, or spicy food).
Finally, surgery may be used to help relieve complications and symptoms. About 60 percent of those with Crohn’s disease had surgery within two decades of being diagnosed with the disease. Surgery may be used to treat fistulas, life-threatening bleeding, intestinal obstructions, and other symptoms. A surgeon may remove a damaged portion of the GI tract then reconnect the sections that are still healthy. Typically, the surgery results are only temporary since the disease will cause flare ups again, often near the reconnected tissue.
Lifestyle factors including stress management, regular exercise, and relaxation techniques won’t help the disease, but could help deal with the symptoms.
EMS and Crohn's Disease
If you have a patient who knows they have Crohn’s disease and are dealing with the difficult symptoms, or even just have the symptoms without a diagnosis, it’s important to get them to a hospital where more definitive treatment can be provided.
When you take the patient history, you should find out about their symptoms (symptom list, frequency, and severity), and check if they smoke or take anti-inflammatory drugs like NSAIDs (Advil, Motrin, Aleve) since that can make things worse.
When you take the patient history, you should find out about their symptoms (symptom list, frequency, and severity), and check if they smoke or take anti-inflammatory drugs like NSAIDs (Advil, Motrin, Aleve) since that can make things worse.
Sources & More Information
Crohn’s & Colitis, “Understanding Crohn’s Disease” https://www.crohnsandcolitis.com/crohns
Mayo Clinic, “Crohn’s disease” https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304
National Institute of Diabetes and Digestive and Kidney Diseases, “Crohn’s Disease” https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease
Mayo Clinic, “Crohn’s disease” https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304
National Institute of Diabetes and Digestive and Kidney Diseases, “Crohn’s Disease” https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease

