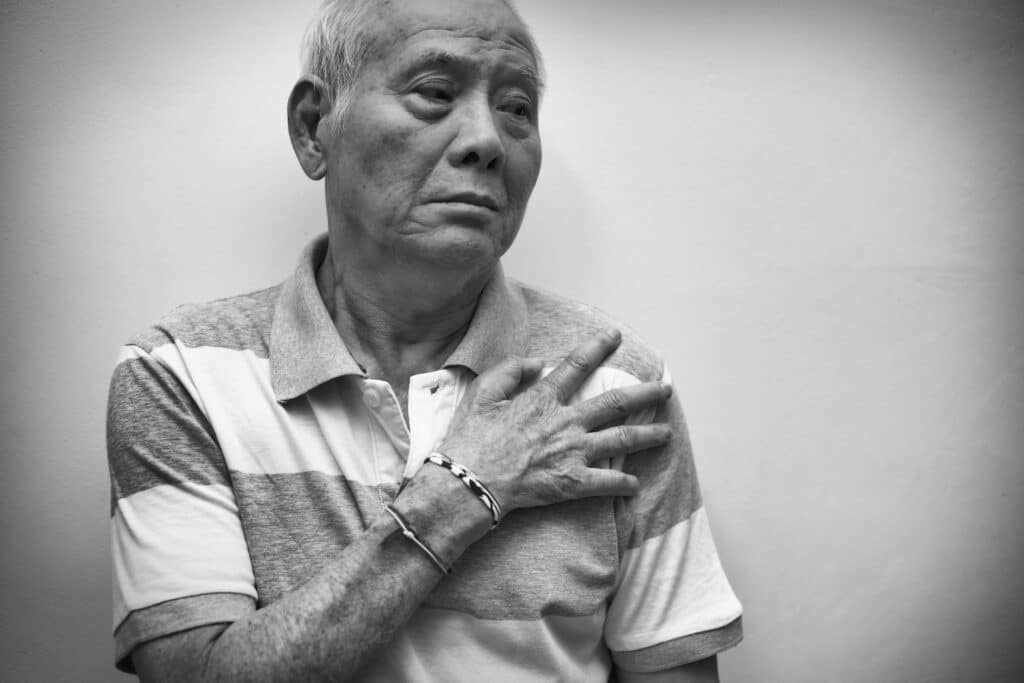
The ER doors slid open automatically as paramedics wheeled in a 78-year-old man. He looked tired and grimacing with pain. His worried daughter walked alongside the stretcher.
His story was that within the past couple of weeks, he had a fairly rapid onset of pain in his shoulders and pelvic area. He was particularly stiff and sore in the mornings. He told me, he thought it was just (osteo) arthritis as he was getting older, but I thought the rapid onset and increasing severity made this unlikely.
He had been taking ibuprofen but it no longer seemed to help. He noticed mild swelling of his wrists and knees in the past few days, and was feeling increasingly fatigued. Just getting out of bed in the last couple of days took great effort, and he was having difficulty dressing himself due to the pain and stiffness.
This morning he couldn’t get out of bed at all, so his daughter called for an ambulance. He denied rashes, fever/chills, headache, or visual disturbances. He had no past history of anything similar. He was generally quite healthy and on no medications. He had Celiac Disease, but was well-controlled on a gluten-free diet.
On exam, his vitals were BP 140/82, P 76, and RR 16. His oral temperature was 99.0 degrees Fahrenheit.
There was no erythema of the joints and only mild swelling of the knees and wrists. His shoulders and hips had decreased active and passive range of motion with tenderness to palpation. His exam was otherwise unremarkable.
Lab studies were normal except for a markedly elevated ESR and CRP. Based on his presentation and lab results, I started him on Prednisone for Polymyalgia Rheumatica.
Polymyalgia Rheumatica (PMR) is an immune-mediated inflammatory disorder that primarily affects people older than age 50. Incidence is about 50/100,000 per year.
The immune system gets abnormally activated and this results in inflammation of the proximal musculoskeletal structures bilaterally, particularly the shoulders, hips, and trunk with rapid onset. The symptoms are worse in the morning and may persist for hours into the day.
Exam findings usually include shoulder tenderness and decreased range of motion. There is usually no erythema, heat, or effusion of the joints, although sometimes there may be some mild swelling of the wrists, MCP joints, and knees. Malaise, mild fever, anorexia, weight loss and depression can accompany the musculoskeletal symptoms. The ESR and CRP will be elevated.
These patients will get dramatic improvement with Prednisone, sometimes within hours of the first dose which helps confirm the diagnosis. The disease does not cause any damage to joints or muscles but, some patients, about 15-20%, develop Giant Cell Arteritis, which can lead to permanent loss of vision. GCA can present with or without PMR symptoms.
Typically, GCA presents with either a new onset headache (usually temporal artery tenderness also), visual disturbance, or jaw claudication. Sometimes systemic symptoms such as malaise and high-spiking fevers can occur.
Diagnosis of GCA is with a temporal artery biopsy. Unfortunately, this can take time to arrange, so often Prednisone will be started empirically while waiting for this test.
Fortunately, our patient did not have any signs or symptoms of GCA. His PMR symptoms responded rapidly to Prednisone. The next morning he was able to get out of bed and get dressed with almost no pain. He had a follow-up with a rheumatologist and was treated with a tapering dose of Prednisone over several months with no relapse.

