Prevalence and Causes
Roughly 1 in 5 adults has a mental illness, making it one of the most common health concerns in the United States. While the vast majority of people with a mental health concern are able to manage their illness well with community support, therapy, and medication, others may eventually experience a “mental health crisis” and need to be treated in an acute or emergent setting. These crises are often when we as EMS providers enter the picture.
Patients experiencing a mental health crisis often end up being seen by EMS either through a request for transfer between facilities or through a 911 response in the community. Since a large percentage of our population lives with the risk of experiencing a mental health crisis, I think that a discussion of some of the common signs, causes, and de-escalation strategies may be helpful.
Depending on how you as an EMS provider come to interact with the patient, be it a scheduled transfer or a 911 response, you may not be aware that your patient has a mental health chief complaint before interacting with them. Because a mental health crisis may be brought on by a very broad range of underlying conditions, there is a correspondingly broad range of signs and symptoms that the patient may be displaying when experiencing a crisis. Patients may be feeling or displaying signs of panic or anxiety, be engaging in bizarre behavior or speech or may have destructive behaviors or feelings toward themselves or others. Some common triggers of a crisis include changes in a relationship, loss of a pet, home or job, real or perceived discrimination, a missed medication dose or drug or alcohol use. A thorough history is important in determining what triggered the crisis state and should be obtained whenever possible.
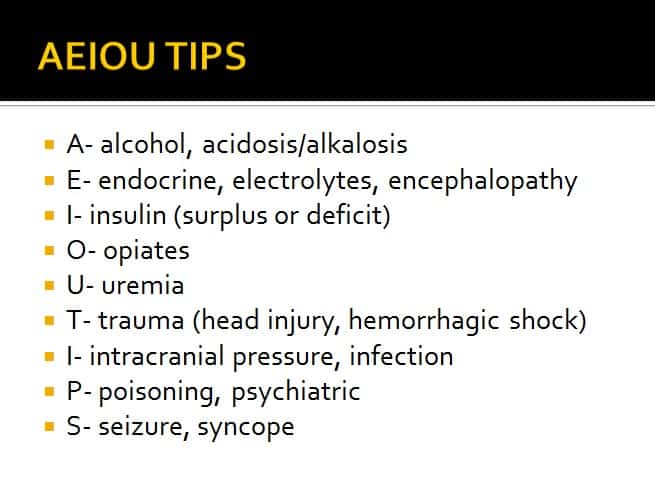
While this article focuses on how to engage a patient experiencing a mental health crisis caused by an underlying psychiatric condition, it is important to remember that these signs and symptoms may also have a physical rather than mental cause. The acronym AEIOU TIPS is useful in keeping different causes of altered mental status in mind (see Image 1).
When dealing with a patient having a crisis, remember to put your safety first. If the scene is not safe, retreat to a secure location until law enforcement can intervene. Even after the scene has been declared safe, be mindful that the patient’s mood may change from calm to violent at a moment’s notice once in your care. Soft restraints or chemical sedation may be warranted if this becomes the case. In some instances, soft restraints may be placed on the patient preemptively at the care provider’s discretion.
Therapeutic Communication
Learning to communicate effectively with someone experiencing a mental health crisis will be invaluable in calming your patient and keeping them from escalating during transport or assessment. As with all of our patients, speaking calmly and honestly is a good first step.
Remember also to:
- Keep a safe distance in case they try to lunge. A distance of at least 2 arm lengths is recommended.
- Do not block their exit as this may cause them to feel trapped.
- Try to match their body position. If they are sitting try to sit or kneel, if they are standing try to stand. Avoid closed off body language such as crossing your arms.
- Inform them well in advance of any actions you will take, especially if it will involve you or someone else touching them.
- It is okay to gently disagree with any delusions that they may have. Reassuring them that, for example, the voices in their head are not real may have a calming effect.
- When asking questions listen fully to the response and repeat it back to them to make sure that you are both on the same page. This action will also show that you are truly listening. Also, try to avoid overstimulation by having one provider do most of the communicating.
- Validate the patient’s feelings but set limits on the patient’s behavior and stick to them.
Resources for Patients and Families
EMS presence will hopefully improve the situation for someone who is experiencing a mental health crisis, but longer term resources may be necessary to help the patient and their family or friends cope. Some valuable resources include the National Alliance on Mental Illness and the Minnesota Department of Human Services, among others (links to websites that have lists of services are at the end of this article). Services available include 24 hour help lines, crisis intervention teams consisting of mental health professionals that can respond to a scene, crisis stabilization teams that help implement a treatment plan in the person’s home, and specialized law enforcement officers trained to respond to mental health crises.
References and Helpful Links
– De-escalation: How To. Trauma Education: The Next Generation. Health Partners. 9-17-15
– Crisis Booklet for adults: https://www.namihelps.org/Crisis-Booklet-Adults.pdf
– Mental Health by the Numbers: https://www.nami.org/Learn-More/Mental-Health-By-the-Numbers
– S Hopkins J Lockwood. The Patient with an Altered Mental Status. ECRN Mod IV Advocate Condell Medical Center. 2009. Accessed online 1-5-15: https://slideplayer.com/slide/3729219


