Overview
Huntington’s disease is an autosomal dominant genetic disease causing a breakdown of nerve cells in the brain, resulting in decline of a person’s physical and mental abilities. Most commonly, Huntington’s disease emerges during adulthood when someone is in their 30s or 40s. When there are signs earlier than that, it is considered juvenile Huntington’s disease, and progresses faster than in adults, becoming fatal 10-15 years after symptoms first appear.
The disease is fatal, with no known cure, and progresses over time so symptoms become more severe. Typically, adults showing signs and symptoms of Huntington’s disease will survive another 15-20 years.
It’s estimated that Huntington’s disease affects 3 to 7 people per 100,000, specifically those of European ancestry. It is less common among other populations such as Japanese, Chinese, and African.
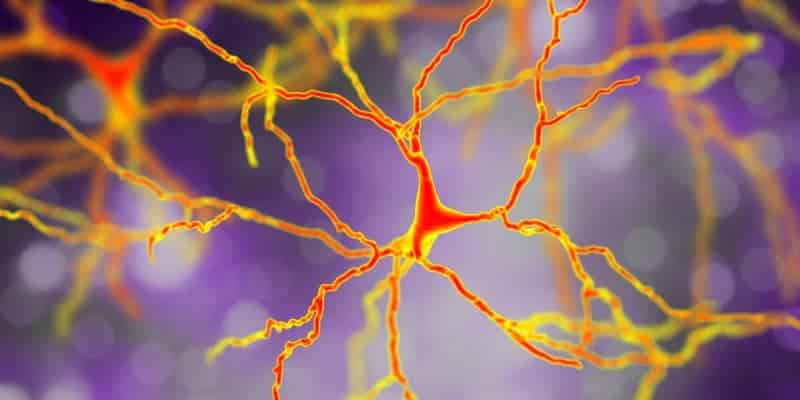
Since it’s a genetic disease, it is most often diagnosed in people who have an affected parent; however, rarely, it can show up in someone who does not have a parent with the disease. It is a result of mutations in the HTT gene, which gives the instructions for making the protein called huntingtin. At this point, the specific function of huntingtin is not known, but it plays a vital role in nerve cells in the brain.
The huntingtin protein becomes an abnormally long version in people who have Huntington’s disease, and then it becomes cut into smaller fragments that cluster in neurons, which disrupts their function and leads to their eventual death. This is how the signs and symptoms of the disease develop.
The disease is fatal, with no known cure, and progresses over time so symptoms become more severe. Typically, adults showing signs and symptoms of Huntington’s disease will survive another 15-20 years.
It’s estimated that Huntington’s disease affects 3 to 7 people per 100,000, specifically those of European ancestry. It is less common among other populations such as Japanese, Chinese, and African.
Since it’s a genetic disease, it is most often diagnosed in people who have an affected parent; however, rarely, it can show up in someone who does not have a parent with the disease. It is a result of mutations in the HTT gene, which gives the instructions for making the protein called huntingtin. At this point, the specific function of huntingtin is not known, but it plays a vital role in nerve cells in the brain.
The huntingtin protein becomes an abnormally long version in people who have Huntington’s disease, and then it becomes cut into smaller fragments that cluster in neurons, which disrupts their function and leads to their eventual death. This is how the signs and symptoms of the disease develop.
Signs and Symptoms
The signs and symptoms present in both cognitive and physical difficulties, which get worse as the disease progresses. The initial symptoms can vary greatly in severity and presentation, and even the course of the disease can present differently in different people.
The signs and symptoms can be split into cognitive/psychiatric disorders, and movement disorders. Some of the cognitive/psychiatric disorders include:
Juvenile Huntington’s disease presents with behavioral changes (such a sudden drop in academic performance or behavioral changes) and physical changes (dystonia affecting gait, problems with writing and fine motor skills, seizures, and tremors).
Once symptoms appear, they will continue becoming more severe as the disease progresses until death (often due to pneumonia or injuries from falls). Late stage Huntington’s disease, when the individual may be confined to a bed and unable to speak, may last as long as 10 years.
The signs and symptoms can be split into cognitive/psychiatric disorders, and movement disorders. Some of the cognitive/psychiatric disorders include:
- Difficulty focusing on tasks
- Tendency to get “stuck” on one thought, behavior, or action – can result in obsessive-compulsive disorder (OCD)
- Loss of impulse control and awareness of one’s own behavior
- Slow to process thoughts and find words
- Trouble with learning new information
- Depression as a result of changes in brain function
- Social withdrawal, insomnia, fatigue, thoughts of death or suicide
- Bipolar disorder
- Chorea, which is involuntary jerking/writhing
- Dystonia, which is problems with muscles including rigidity or contracted muscles
- Eye movements that are abnormal (including slow)
- Impaired walk, balance, or posture
- Struggle with the physicality of speech and swallowing
Juvenile Huntington’s disease presents with behavioral changes (such a sudden drop in academic performance or behavioral changes) and physical changes (dystonia affecting gait, problems with writing and fine motor skills, seizures, and tremors).
Once symptoms appear, they will continue becoming more severe as the disease progresses until death (often due to pneumonia or injuries from falls). Late stage Huntington’s disease, when the individual may be confined to a bed and unable to speak, may last as long as 10 years.
Prevention and Diagnosis
Those with a known family history of Huntington’s disease may consider genetic testing as they make plans to have children. The genetic test can identify if the parent could develop the disease, and also do prenatal genetic testing to look for the gene mutation. They could choose to do in vitro fertilization and preimplantation genetic diagnosis, which means eggs would be removed and fertilized in a laboratory, then tested for the presence of the gene mutation. Only the embryos without the gene would be implanted in the mother’s uterus.
When seeing a doctor for a diagnosis, the diagnosis is first based on the patient’s answers to questions, a physical exam with a review of the family’s medical history, and additional psychiatric and neurological tests.
In a neurological examination, the doctor may check motor symptoms, sensory symptoms (such as sense of touch, vision, and hearing), and psychiatric symptoms (like mood). Psychiatric testing includes assessing the patient’s memory, reasoning abilities, mental agility, language, and spatial reasoning. Based on these findings, the patient may be referred to a psychiatrist for a more comprehensive psychiatric evaluation.
Brain-imaging tests may be ordered to assess the brain with an MRI and CT scan that could show structural changes in the parts of the brain that are affected by Huntington’s disease. Brain changes may not be obvious early on in the disease.
If the doctor is considering a Huntington’s disease diagnosis, the final step may be a gene test, particularly in someone who does not have a family history of the disease.
When seeing a doctor for a diagnosis, the diagnosis is first based on the patient’s answers to questions, a physical exam with a review of the family’s medical history, and additional psychiatric and neurological tests.
In a neurological examination, the doctor may check motor symptoms, sensory symptoms (such as sense of touch, vision, and hearing), and psychiatric symptoms (like mood). Psychiatric testing includes assessing the patient’s memory, reasoning abilities, mental agility, language, and spatial reasoning. Based on these findings, the patient may be referred to a psychiatrist for a more comprehensive psychiatric evaluation.
Brain-imaging tests may be ordered to assess the brain with an MRI and CT scan that could show structural changes in the parts of the brain that are affected by Huntington’s disease. Brain changes may not be obvious early on in the disease.
If the doctor is considering a Huntington’s disease diagnosis, the final step may be a gene test, particularly in someone who does not have a family history of the disease.
Treatment
Since there is no cure, treatment is focused on easing the signs and symptoms as much as possible, but cannot prevent the progression of the disease. The medications are based on the symptoms, such as for movement disorders and psychiatric disorders. Drugs can help suppress the movements to help chorea, but can also have unwanted side effects making other symptoms worse. Antidepressants, antipsychotics, and mood-stabilizing drugs may be prescribed based on what signs and symptoms are present.
An individual with Huntington’s disease may get psychotherapy to help cope with the behavioral problems and dealing with the disease. A speech therapist can help with improving the ability to speak, swallow, and communicate effectively. Physical therapy provides exercises to maintain mobility as long as possible. Occupational therapy assists the individual with the disease and the family to utilize assistive devices to improve functional abilities for as long as possible.
It is recommended that anyone diagnosed with Huntington’s disease utilize support services and therapists to cope with the fatal disease. There will also need to be planning for end-of-life care in the advanced stages of the disease, including legal documents and hospice care.
An individual with Huntington’s disease may get psychotherapy to help cope with the behavioral problems and dealing with the disease. A speech therapist can help with improving the ability to speak, swallow, and communicate effectively. Physical therapy provides exercises to maintain mobility as long as possible. Occupational therapy assists the individual with the disease and the family to utilize assistive devices to improve functional abilities for as long as possible.
It is recommended that anyone diagnosed with Huntington’s disease utilize support services and therapists to cope with the fatal disease. There will also need to be planning for end-of-life care in the advanced stages of the disease, including legal documents and hospice care.
Sources and More Information
Huntington’s Disease Society of America, “Overview of Huntington’s Disease” https://hdsa.org/what-is-hd/overview-of-huntingtons-disease/
Mayo Clinic, “Huntington’s disease” https://www.mayoclinic.org/diseases-conditions/huntingtons-disease/symptoms-causes/syc-20356117
National Institute of Neurological Disorders and Stroke, “Huntington’s Disease Information Page” https://www.ninds.nih.gov/Disorders/All-Disorders/huntingtons-Disease-Information-Page
US National Library of Medicine, Genetics Home Reference, “Huntington disease” https://ghr.nlm.nih.gov/condition/huntington-disease#genes
Mayo Clinic, “Huntington’s disease” https://www.mayoclinic.org/diseases-conditions/huntingtons-disease/symptoms-causes/syc-20356117
National Institute of Neurological Disorders and Stroke, “Huntington’s Disease Information Page” https://www.ninds.nih.gov/Disorders/All-Disorders/huntingtons-Disease-Information-Page
US National Library of Medicine, Genetics Home Reference, “Huntington disease” https://ghr.nlm.nih.gov/condition/huntington-disease#genes


