Overview
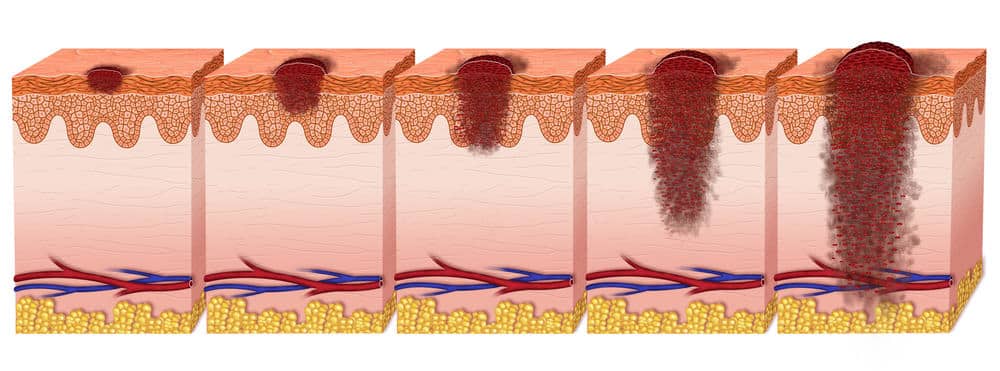
Ever been worried about a new mole or discoloration appearing on your skin? Welcome to melanoma, the most serious form of skin cancer, which is increasing in people under 40. Almost 200,000 new cases of melanoma are estimated to be diagnosed in America this year – of those cases, 35% will be invasive, meaning they penetrate through to the second layer of skin.
While melanoma is less common than other forms of skin cancer, it’s known for how fast it grows and spreads. Cancer occurs when there is an overgrowth of cells in the body – in melanoma, these cells are skin cells. Melanocytes are skin cells that make a brown pigment called melanin, which colors the skin. A tan is formed when skin is exposed to the sun, and melanocytes make more pigment as it protects the deeper layers of skin from the sun.
While the exact cause of melanoma isn’t known, it’s suspected that UV radiation from sunlight or tanning beds/lamps increases the risk of melanoma from damaging cell DNA, which is why it’s recommended to always use sunscreen and limit sun exposure.
While melanoma is less common than other forms of skin cancer, it’s known for how fast it grows and spreads. Cancer occurs when there is an overgrowth of cells in the body – in melanoma, these cells are skin cells. Melanocytes are skin cells that make a brown pigment called melanin, which colors the skin. A tan is formed when skin is exposed to the sun, and melanocytes make more pigment as it protects the deeper layers of skin from the sun.
While the exact cause of melanoma isn’t known, it’s suspected that UV radiation from sunlight or tanning beds/lamps increases the risk of melanoma from damaging cell DNA, which is why it’s recommended to always use sunscreen and limit sun exposure.
Signs and Symptoms
Typically, a new mole or change in an existing mole is the first sign of melanoma. Moles are a normal skin mark, and most people have 10-45 moles that develop or disappear over time. The acronym ABCDE explains warning signs to look for in moles:
While melanoma is often a change in an existing mole or a new mole, it can appear without that type of pigmentation on skin that looks relatively normal.
Melanoma can develop anywhere on the body, but are most often found on areas that have direct exposure to the sun (back, arms, face, legs). Men will more typically experience melanoma in the trunk, head, and neck, while women most often form melanoma on the arms and legs.
Melanoma can be found on areas that don’t receive very much sun exposure (like the bottom of the feet, under the fingernails, or on genitalia), and these types of hidden melanomas are more common in people with darker skin.
Skin self-exams are recommended for people to do at home using a full-length mirror and hand-held mirror. Any areas of skin that has changed are recommended to be checked by a doctor. A skin exam can also be performed by a doctor as part of a regular health check.
- A: Asymmetry – if both sides of the mole don’t match each other
- B: Border – if the edges of the mole are not smooth
- C: Color – it includes multiple shades and uneven color
- D: Diameter – any change in size of a mole
- E: Evolving – the mole has changed within the last few months
While melanoma is often a change in an existing mole or a new mole, it can appear without that type of pigmentation on skin that looks relatively normal.
Melanoma can develop anywhere on the body, but are most often found on areas that have direct exposure to the sun (back, arms, face, legs). Men will more typically experience melanoma in the trunk, head, and neck, while women most often form melanoma on the arms and legs.
Melanoma can be found on areas that don’t receive very much sun exposure (like the bottom of the feet, under the fingernails, or on genitalia), and these types of hidden melanomas are more common in people with darker skin.
Skin self-exams are recommended for people to do at home using a full-length mirror and hand-held mirror. Any areas of skin that has changed are recommended to be checked by a doctor. A skin exam can also be performed by a doctor as part of a regular health check.
Risk Factors
There are many risk factors for melanoma; however, having these risk factors does not guarantee someone will develop melanoma, since the exact cause still isn’t known.
Those with a fair complexion that burns easily and doesn’t tan, with blue or light-colored eyes, and red or blonde hair are more at risk for melanoma. Having a history of severe (blistering) sunburns, especially while growing up, creates a higher risk of melanoma. This includes being exposed to natural or artificial sunlight (UV radiation) for long or repeated stretches of time, such as living closer to the equator or at a higher elevation.
Those with many large or small moles are considered to have a higher chance of developing melanoma, along with having a family history of unusual moles. There does seem to be a genetic link since those with a family history of melanoma (a close relative such as a parent) are more likely to develop it.
Those with a fair complexion that burns easily and doesn’t tan, with blue or light-colored eyes, and red or blonde hair are more at risk for melanoma. Having a history of severe (blistering) sunburns, especially while growing up, creates a higher risk of melanoma. This includes being exposed to natural or artificial sunlight (UV radiation) for long or repeated stretches of time, such as living closer to the equator or at a higher elevation.
Those with many large or small moles are considered to have a higher chance of developing melanoma, along with having a family history of unusual moles. There does seem to be a genetic link since those with a family history of melanoma (a close relative such as a parent) are more likely to develop it.
Prevention
While there are many risk factors for developing melanoma, the best way to prevent it is avoiding extended direct sun exposure – in North America, people should avoid the sun betwen 10am-4pm, which is when the rays are the strongest. Clouds don’t offer protection from UV rays, so you could get UV radiation even on a cloudy day.
Sunscreen doesn’t prevent UV radiation completely; however, it does help limit the harmful exposure. Dermatologists recommend using a broad-spectrum, water-resistant, SPF of at least 30 sunscreen, and re-applying every two hours when in the sun.
Protective clothing helps protect from UV rays, especially when combined with sunscreen. Wear a broad-rimmed hat (more coverage than a baseball cap) and cover your arms and legs with tightly woven clothing – activewear companies often sell garments that are meant for sun protection and are lightweight. Sunglasses that block UV radiation (both UVA and UVB rays) are always recommended.
Being familiar with your skin, by performing regular skin checks, will help you notice any changes faster, so a doctor can also check any changes in pigmentation. Since melanoma spreads rapidly, it’s best to treat it as soon as possible.
Sunscreen doesn’t prevent UV radiation completely; however, it does help limit the harmful exposure. Dermatologists recommend using a broad-spectrum, water-resistant, SPF of at least 30 sunscreen, and re-applying every two hours when in the sun.
Protective clothing helps protect from UV rays, especially when combined with sunscreen. Wear a broad-rimmed hat (more coverage than a baseball cap) and cover your arms and legs with tightly woven clothing – activewear companies often sell garments that are meant for sun protection and are lightweight. Sunglasses that block UV radiation (both UVA and UVB rays) are always recommended.
Being familiar with your skin, by performing regular skin checks, will help you notice any changes faster, so a doctor can also check any changes in pigmentation. Since melanoma spreads rapidly, it’s best to treat it as soon as possible.
Diagnosis
Melanoma is best diagnosed with a biopsy, after a doctor has examined an area of skin that looks like it could be cancerous. There are different types of biopsies: punch biopsy (using a blade to remove a circular patch of skin, which could be the entire mole), excisional biopsy (the entire mole/growth is removed along with a bit of normal skin), and incisional biopsy (only the irregular part of a mole is removed).
If a diagnosis of melanoma is confirmed with the biopsy, then the stage of cancer has to be determined. Thickness of the melanoma dictates the stage of the cancer – the thicker the tumor is, the more severe the cancer. A doctor will also check to see if the melanoma has spread at all using a sentinel node biopsy – the area where the melanoma was removed is injected with a dye that goes into the lymph nodes. If those lymph nodes are cancer-free, then it’s likely the cancer has not spread.
A doctor will also check for other signs of the severity of a melanoma (how many cancer cells are found or if there’s an open sore). Stage I melanoma is small with a high success rate from treatment. Stage IV melanoma means the cancer has spread to internal organs.
If a diagnosis of melanoma is confirmed with the biopsy, then the stage of cancer has to be determined. Thickness of the melanoma dictates the stage of the cancer – the thicker the tumor is, the more severe the cancer. A doctor will also check to see if the melanoma has spread at all using a sentinel node biopsy – the area where the melanoma was removed is injected with a dye that goes into the lymph nodes. If those lymph nodes are cancer-free, then it’s likely the cancer has not spread.
A doctor will also check for other signs of the severity of a melanoma (how many cancer cells are found or if there’s an open sore). Stage I melanoma is small with a high success rate from treatment. Stage IV melanoma means the cancer has spread to internal organs.
Treatment
For early-stage melanoma, surgery removes the melanoma from the skin. A small, thin melanoma may simply require a biopsy to remove it and no further treatment. More aggressive melanoma may require removal of more skin around the affected area and tissue beneath the skin.
When melanoma has spread beyond just the skin, there could be surgery removing affected lymph nodes, chemotherapy (to destroy the cancer cells), radiation therapy (often used after surgery removing lymph nodes to destroy remaining cancer cells), biological therapy (boosts immune system to encourage the body to fight off the cancer), and targeted therapy (medications to fight cancer cells).
While treatment can be successful in destroying the cancer cells, there is a risk of cancer coming back (recurrent cancer). Melanoma is a cancer that may never go away for some people, and they have to continue treatment.
After completing melanoma treatment, the patient will still be monitored closely due to the risk of melanoma coming back – people who have had melanoma have a higher risk of developing it again.
When melanoma has spread beyond just the skin, there could be surgery removing affected lymph nodes, chemotherapy (to destroy the cancer cells), radiation therapy (often used after surgery removing lymph nodes to destroy remaining cancer cells), biological therapy (boosts immune system to encourage the body to fight off the cancer), and targeted therapy (medications to fight cancer cells).
While treatment can be successful in destroying the cancer cells, there is a risk of cancer coming back (recurrent cancer). Melanoma is a cancer that may never go away for some people, and they have to continue treatment.
After completing melanoma treatment, the patient will still be monitored closely due to the risk of melanoma coming back – people who have had melanoma have a higher risk of developing it again.
Sources and More Information
American Academy of Dermatology Association, “Melanoma” https://www.aad.org/public/diseases/skin-cancer/melanoma
American Cancer Society, “Melanoma Skin Cancer” https://www.cancer.org/cancer/melanoma-skin-cancer.html
Mayo Clinic, “Melanoma” https://www.mayoclinic.org/diseases-conditions/melanoma/symptoms-causes/syc-20374884
Skin Cancer Foundation, “Melanoma” https://www.skincancer.org/skin-cancer-information/melanoma
U.S. National Library of Medicine – MedlinePlus, “Melanoma” https://medlineplus.gov/melanoma.html
American Cancer Society, “Melanoma Skin Cancer” https://www.cancer.org/cancer/melanoma-skin-cancer.html
Mayo Clinic, “Melanoma” https://www.mayoclinic.org/diseases-conditions/melanoma/symptoms-causes/syc-20374884
Skin Cancer Foundation, “Melanoma” https://www.skincancer.org/skin-cancer-information/melanoma
U.S. National Library of Medicine – MedlinePlus, “Melanoma” https://medlineplus.gov/melanoma.html


