A stoic 73-year-old man was brought to the ED with dyspnea. He had a history of COPD and was administered albuterol en route to the hospital with no change in dyspnea.
I noticed his shoes were not tied. He said the difficulty breathing had come on over the past day or so and was worse if laying down or bending forward. He denied any fever or increased cough. He had been using his usual inhalers at home without improvement. His oxygen saturation was 93% and he was on oxygen at a rate of 4 liters per minute.
A review of his systems was positive for difficulty with urination. He admitted he had been having increasing problems emptying his bladder to the point where he could only pass a few drops if that. Other than mild tachypnea, his vital signs were normal. Auscultation of the chest revealed some mild end-expiratory wheezes and crackles bilaterally.
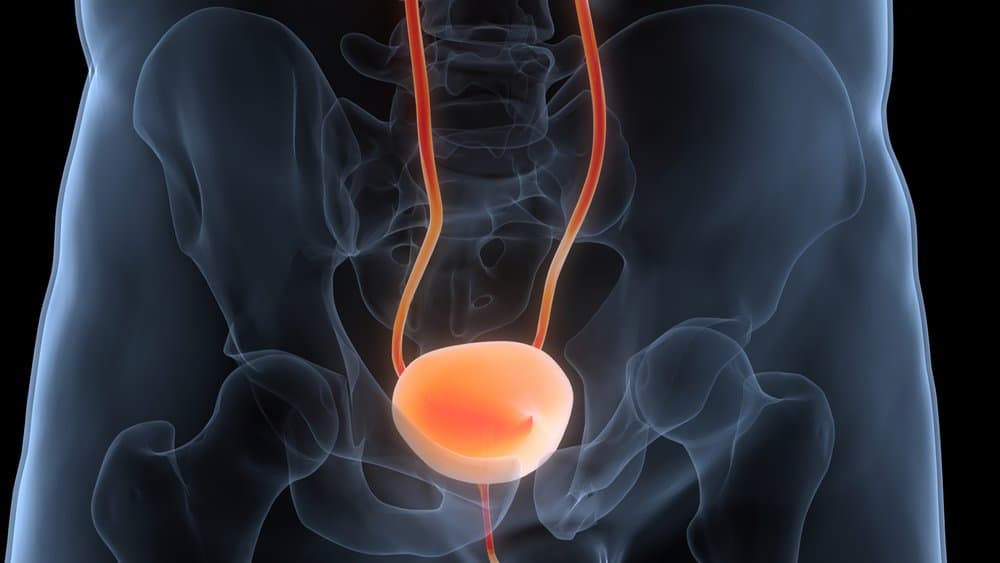
He had 2+ ankle edema which he said had come on over the past few days. He had distention of his abdomen due to a large palpable mass. A rectal exam revealed an enlarged non-tender prostate. A bedside ultrasound of his abdomen showed an extremely distended bladder.
A urinary catheter was placed immediately, which started draining a large volume of bloody urine. (Blood was due to bladder injury from overstretching.) By the following day, he “felt like a new man.” The catheter had drained over 6 liters. His dyspnea resolved as did his edema.
This patient was dyspneic for two reasons: he was fluid overloaded due to post-renal failure, that is lack of kidney function due to urethral obstruction, which was causing fluid to back up and accumulate in his lungs and tissues. Secondly, the large bladder was causing a mechanical restriction of diaphragm movement.
He was discharged home with a foley catheter and an appointment for a urologic consult to arrange a transurethral prostatectomy.
I noticed his shoes were not tied. He said the difficulty breathing had come on over the past day or so and was worse if laying down or bending forward. He denied any fever or increased cough. He had been using his usual inhalers at home without improvement. His oxygen saturation was 93% and he was on oxygen at a rate of 4 liters per minute.
A review of his systems was positive for difficulty with urination. He admitted he had been having increasing problems emptying his bladder to the point where he could only pass a few drops if that. Other than mild tachypnea, his vital signs were normal. Auscultation of the chest revealed some mild end-expiratory wheezes and crackles bilaterally.
He had 2+ ankle edema which he said had come on over the past few days. He had distention of his abdomen due to a large palpable mass. A rectal exam revealed an enlarged non-tender prostate. A bedside ultrasound of his abdomen showed an extremely distended bladder.
A urinary catheter was placed immediately, which started draining a large volume of bloody urine. (Blood was due to bladder injury from overstretching.) By the following day, he “felt like a new man.” The catheter had drained over 6 liters. His dyspnea resolved as did his edema.
This patient was dyspneic for two reasons: he was fluid overloaded due to post-renal failure, that is lack of kidney function due to urethral obstruction, which was causing fluid to back up and accumulate in his lungs and tissues. Secondly, the large bladder was causing a mechanical restriction of diaphragm movement.
He was discharged home with a foley catheter and an appointment for a urologic consult to arrange a transurethral prostatectomy.


